Why is back pain so difficult to treat?
Back pain, including acute and chronic low back pain, is a common problem that interfere's with everyone at some point in their life.
Up to 80% of adults will experience low back pain at least once in their lives and according to one study, the one year prevalence of low back pain in children was reported to be 58%!
Due to the limited objective testing for pain, treating both acute and chronic back pain is one of the most difficult tasks in musculoskeletal medicine.
Most cases of low back pain in children or adults do not have an identifiable disease, injury, or cause.
Research suggests that nearly 80% of cases of low back pain do not have a specific identifiable cause aside from arthritis, abnormal alignment and a lack of physical fitness.
Most back pain is musculoskeletal, which means that it comes from the normal use and strain put on muscles, ligaments, tendons and bones, and most of the time none of these are caused by serious medical conditions.
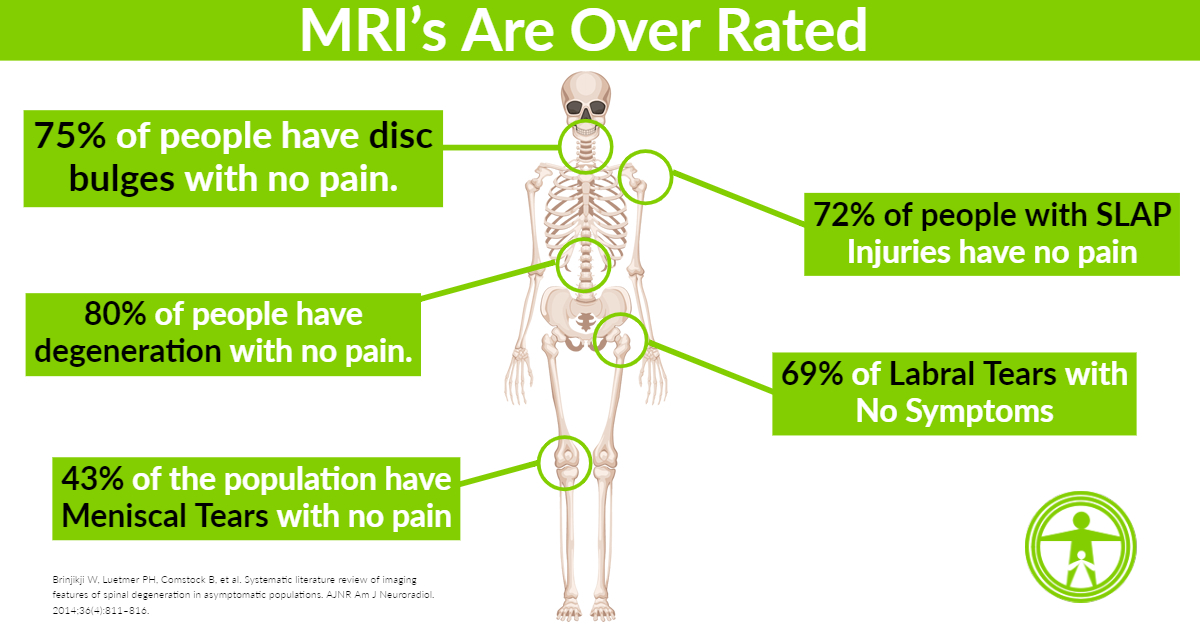
Making things even more complex, the findings you see on Xray, CT or MRI's having nothing to do with how you feel?
MRI Examinations Are (Generally) Useless For Back Pain
In a recent study, scientists discovered that the majority of people who get advanced imaging studies have all sorts of degeneration, arthritis, tears and herniation's and yet no symptoms.
In other words, just because you have a disc herniation, that doesn't mean it's what's causing your pain.
From the authors mouth:
“Advanced imaging (MRI and CT) are increasingly used in the evaluation of patients with low back pain. Findings such as disk degeneration, facet hypertrophy, and disk protrusion are often interpreted as causes of back pain, triggering both medical and surgical interventions, which are sometimes unsuccessful at alleviating the patient's symptoms.” (Brinjikji, et al., 2015, p.811)
The key results of this systematic review were (Brinjikji et al., 2015, p. 811-812):
- The prevalence of disc degeneration ranged from 37% in asymptomatic individuals in their 20s to 96% of those in their 80s.
- Disc signal loss was present in over 50% of individuals older than 40 years and by 60 years, 86% of individuals had signal loss of scans.
- Disc height loss and disc bulges increased on average 1% per year.
- Disc protrusions and annular fissures did not substantially increase with age.
- Facet joint degeneration is rare below 40 years of age and the prevalence increases sharply with ages over 40 years.
- Spondylolisthesis is not commonly found in asymptomatic individuals until 60 years of age but prevalence doesn't increase greatly until 70-80 years.
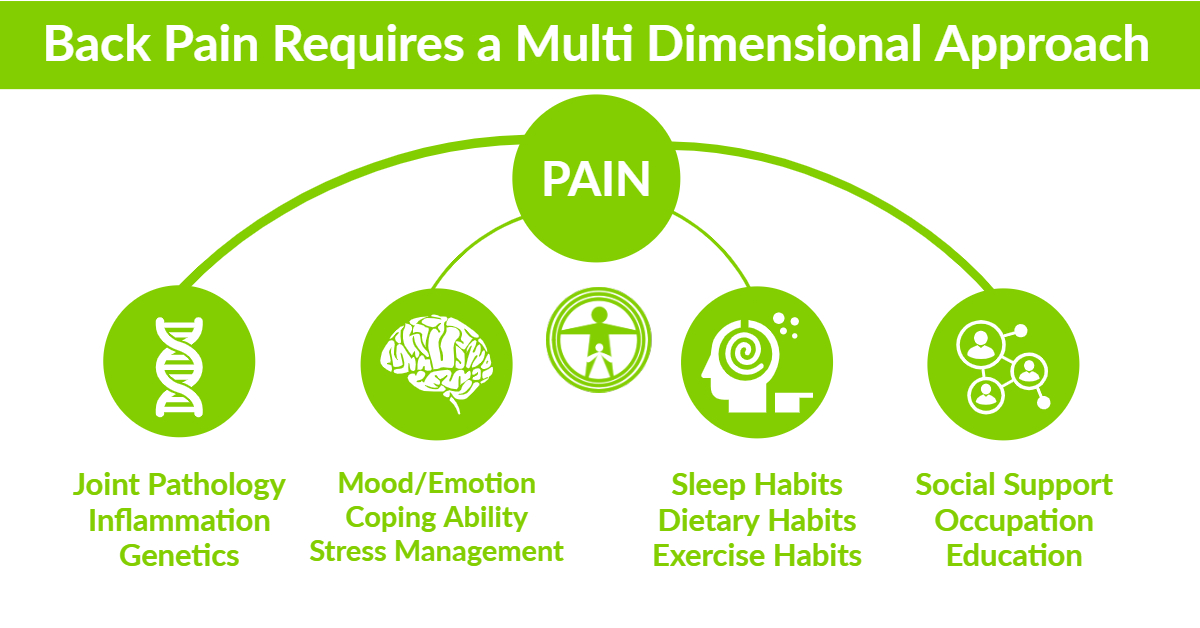
Solving Back Pain Requires a Multi-Dimensional Approach
The most important step to solving back pain is to of course rule out any serious pathology.
Quite honestly, the best way to do this is with a low cost, non-invasive and immediate interpretation of your condition utilizing digital x-rays.
Generally, Xrays are an excellent way to assess your back pain and rule out most of the serious stuff.
Improve Your Personal Fitness
The next step is to begin improving how you move. This includes correcting posture, abnormal spine alignment and improving range of motion and flexibility. This is why a functional movement assessment is important.
If you cannot do the basics of squatting, lunging, bending forward, backward, etcs, then these are basic movements that need to be addressed.
Exercise is the foundation of chronic back pain treatment and it includes flexibility, mobility, strength and rest.
Improve Your Personal Diet & Nutrient Status
On top of making sure that you are at least doing the minimal amount of movement required to be healthy, the next step to focus on is your diet.
Some diets are highly inflammatory, especially those high in trans fats, refined sugars and processed foods.
If you need help optimizing your diet or improving personal nutrition, then consider my Functional Medicine services.
The best diet that I can recommend is the Paleo Diet or Whole30. Not only do these diets help you to keep inflammation down, but they also help to maintain a healthy weight which could also help lessen your back pain by reducing the pressure on your spine.
Improve Your Personal Relationship With Yourself
Chronic back pain is straining both physically and emotionally.
To manage the frustration, irritability, depression and other psychological aspects of dealing with chronic pain, you want to consider seeing a clinical psychologist or look into cognitive behavioral therapy.
This specialist may recommend meditation, yoga, tai chi and other cognitive and relaxation strategies to keep your mind from focusing on pain.
Improve Your Lifestyle
When you have chronic pain, it’s important to pay attention to the activities that you're doing daily.
- Really listen to your body and learn how to be present.
- Take a break from constantly looking down at your phone.
- Work on improving your non-exercise related activity.
- Take it easy on tasks such as carrying groceries such learning how to take several trips when carrying them into your home.
- Take note of the activities that worsen your pain and avoid them if possible.
Not only could this help your back feel better, it could also prevent the underlying condition from advancing.
Another important lifestyle change to try is giving up smoking. Nicotine is scientifically known to accentuate pain and delay healing.
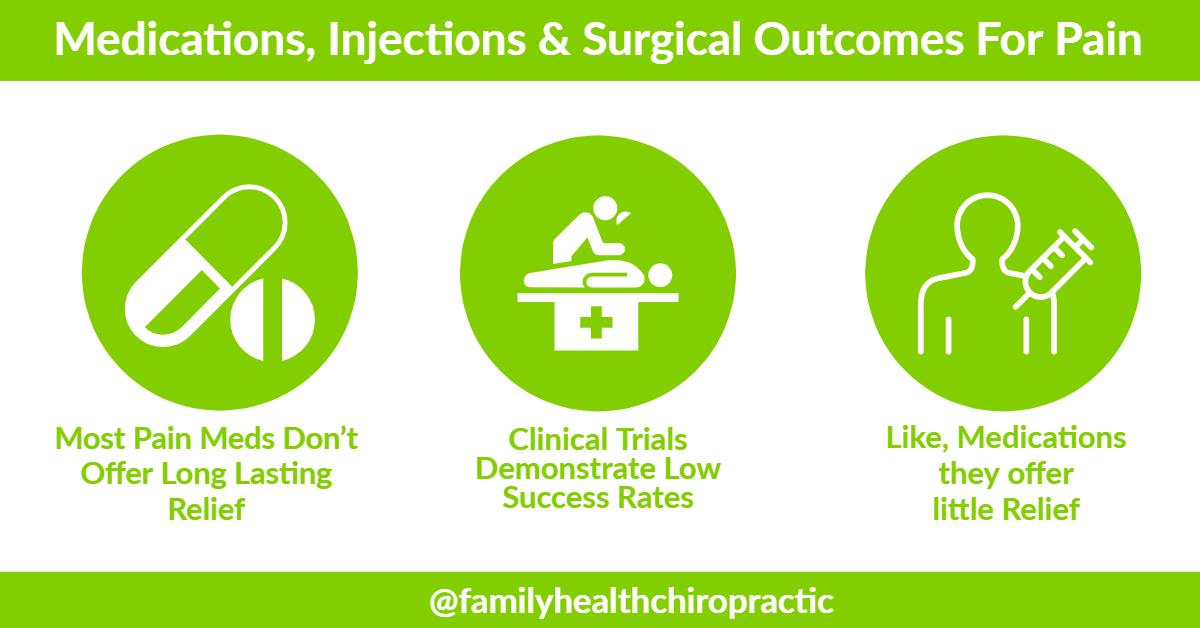
Medications, Injections and Surgery Help, Not Really…
Many of the most popular treatments on offer from doctors for chronic nonspecific low back pain — bed rest, spinal surgery, opioid painkillers, steroid injections — have been proven ineffective in the majority of cases, and sometimes downright harmful.
As of 2016, 14,500 Americans died from opioid-related deaths. Opioid prescribing is common among people with back pain, with almost 20 percent receiving long-term opioid prescriptions.
Here’s what's Crazy: All these opioids were being prescribed before we actually knew if they helped people with chronic lower back pain!!!
Dumb.
It gets worse: Now high-quality evidence is coming in, and opioids don’t actually help many patients with chronic low back pain.
This newly published randomized controlled trial was the first to compare the long-term use of opioids versus non-opioid medications (such as anti-inflammatory drugs and acetaminophen) for chronic low back pain, and hip or knee osteoarthritis.
After a year, the researchers found opioids did not improve patients’ function any more than the non-opioids, and the patients on opioids were actually in slightly more pain compared to the non-opioid group (perhaps the result of “opioid-induced hyperalgesia” — heightened pain brought on by these drugs).
As for surgery, only a small minority of patients with chronic low back pain require it, according to UpToDate, a service that synthesizes the best available research for clinicians.
In randomized trials, there was no clinically meaningful difference when comparing the outcomes of patients who got spinal fusion (which has become more and more popular in the US over the years) with those who got a nonsurgical treatment.
Steroid injections for back pain, another popular medical treatment, tend to have similarly lackluster results: They improve pain slightly in the short term, but the effects dissipate within a few months. They also don’t improve patients’ long-term health outcomes.
Want to Know What Does Work?
- Daily Exercise
- Optimizing Your Diet
- Yoga
- Pilates
- Tai Chi
- Chiropractic/Physical therapy/Massage
Final Thoughts
When it comes to treating acute or chronic low back pain, taking a multi-dimensional approach is the goal.
This means that there isn't a magic bullet when it comes to healing.
There's not 1 adjustment that I can do that can help.
Rather, it's a combination of the things that I try to teach you that will end up helping you achieve the best results.
In February 2017, even the American College of Physicians advised doctors and patients try “non-drug therapies” such as exercise, acupuncture, tai chi, yoga, chiropractic, and avoid prescription drugs or surgical options wherever possible.
This was a recommendation even a year earlier in March 2016, when the Centers for Disease Control and Prevention also came out with new guidelines urging health care providers to turn to non-drug options and non-opioid painkillers before considering stronger medications.