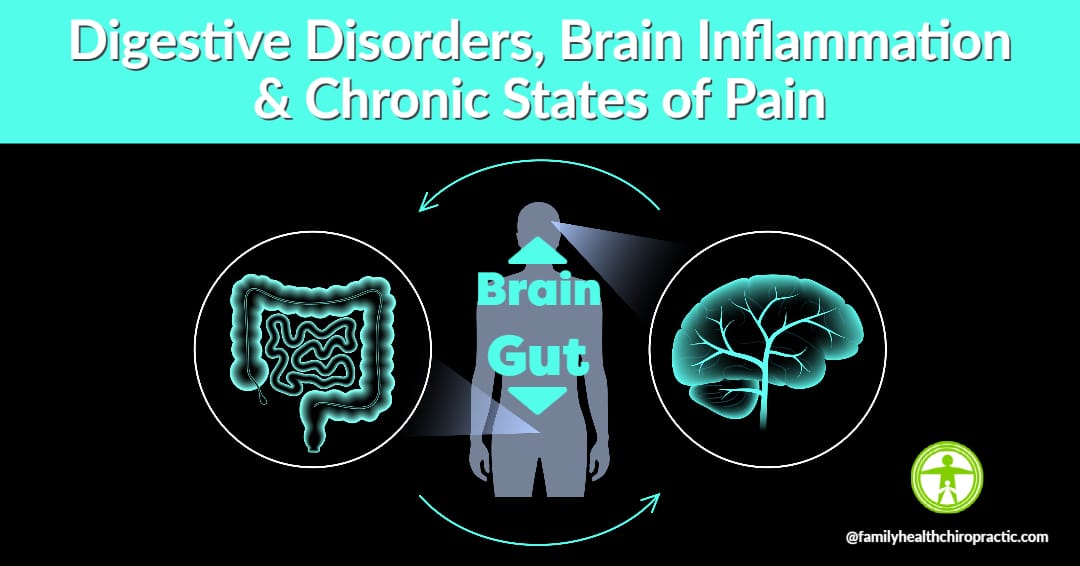
Digestive disorders can cause brain (central nervous system) dysfunction and vice-versa.
Most people innately know one of the most important systems in their body is the brain and spinal cord (central nervous system).
It’s well accepted and understood that the central nervous system controls every major organ, tissue, and cell in the body. Taking care of your spine is crucial because it’s the armor and protection for the spinal cord and nerves. It’s obvious that a damaged spine (osteoarthritis of the vertebrae, degenerative disc disease, altered alignment, nerve impingement, etc.) contributes to ill health, reduced quality of life and longevity.
What isn’t so obvious is that HALF of your nerve cells are in the gut. It’s also not so obvious that most of our serotonin and dopamine are produced within our digestive system. Finally, depending on the research paper you reference, anywhere from 70 to 80% or more of your immune function stems from your digestive system.
So what does this mean for you?
It means that your capacity for feeling and emotional expression, your ability to consume healthy food and fully digest those nutrients for optimal function, your immune system’s ability to protect your body from foreign invaders are all influenced by digestive disorders.
Whether we are talking about “feel good” chemicals that influence mood, depression, fatigue or happiness, hormone regulation to support vitality or neuropeptides and enkephalins, which act as painkillers in the body; the Brain-Gut Axis controls it all.
In this article, I’m going to outline the 7 primary gut pathologies that can break the Brain-Gut axis causing nutrient deficiencies, hormone imbalance, immune dysregulation, brain inflammation (mood and cognitive disorders) and chronic pain.
Chronic Health Conditions are Connected to Digestive Disorders
Almost every chronic health condition or disease is mediated by underlying pathologies of physiological dysfunction that are also connected to digestive disorders.
For example, GERD or Gastro Esophageal Reflux Disease is simply a description of what is going on.
The more important thing to know is that it could be caused by low stomach acid, dysbiosis or imbalances in good and bad bacteria, food sensitivities, parasitic or viral infections.
This is why Functional and Integrative Medicine approach is so important. It's a system that allows us to not simply get a diagnosis, but begin to systematically correct imbalances (improve function) that are causing or will cause disease.
The primary risk factors for developing digestive disorders include:
- Family history
- Cesarean birth
- Formula-fed vs nursed
- Consuming a standard American diet
- Food poisoning
- Antibiotic abuse or overuse
- Other medications
- Chronic stress
- Sleep deprivation
- Physical inactivity/sedentarism
- Hypothyroidism
- HPA-Dysfunction (aka Adrenal Fatigue or Exahustion)
- Excess alcohol consumption
- Cigarette smoking
- Environmental Toxins or Toxic Load
Each of the above mentioned risk factors can all lead to profound alterations in the development and maintenance of the gastrointestinal microbiome and ecosystem.
A Brief Overview of Gut Health and Function
I’m sure you’ve heard the saying, “You are what you eat.” It’s not 100% true.
Eating the right type of food for your body is crucial to optimizing health, but that’s only step number one.
Fully digesting, absorbing and assimilating the nutrients from the food you are eating matters most. And it’s absolutely possible for you to be eating an appropriate diet and still not get all the benefits because of underlying digestive issues.
The GI tract is a hollow tube, starting with the mouth and ending with the anus. And as food makes its way throughout our body, it will encounter several structures including the pharynx, the esophagus, the stomach and intestines, the rectum and accessory organs such as the salivary glands, liver, gallbladder, and pancreas.
All that said, the GI tract has two primary purposes:
- Break food or macronutrients (protein, carbs and fats) down into micronutrients (amino acids, vitamins, minerals, water, etc) which are then absorbed to provide our body with fuel to function.
- Serves as a barrier of protection, protecting us from foreign substances entering our bloodstream and causing problems
Food is certainly the most powerful form of medicine, but if you cannot use the food you are consuming, you cannot get your medicine. The same is true with supplements and even pharmaceuticals.
Aside from mechanical and chemical digestion of food, our digestive system is also home to billions of microbes that influence our health.
We actually have ten times more microbes in the human body than human cells!
These gut microbes are absolutely crucial to your health in that they promote normal GI functions of digestion/absorption, protect against infection, regulate our metabolism, influence hormone production and metabolism and are home to a majority of the immune cells in our body.
An altered gut microbiome is implicated in just about every chronic inflammatory disease, including chronic back pain.
For example, there is a link between the gut and the brain. Problems in the gut, like inflammation, can lead to a higher risk of problems associated with the brain, such as dementia, autism spectrum disorders, neurological conditions, depression and/or anxiety.
The 3 primary functions of our microbiome include:
- Metabolic – the bacteria help to digest the food we eat, create vitamins and compounds that our body requires for normal function
- Structural – short-chain fatty acids (butyrate and propionate) contribute to differentiation of cells and imbalances in the microbiome result in LPS production (highly inflammatory to the gut and brain)
- Protective – the mucosal lining itself is a barrier of protection that contains the gut-associated-lymphoid-tissue (GALT) which makes up most immune cells in our body
The 7 Primary Gut Dysfunctions
There are seven primary gut pathologies that I will cover in this article, and they underlie virtually all gut diseases, syndromes, and symptoms, from IBS to GERD to constipation to inflammatory bowel disease to hemorrhoids.
And this is where you’ll really need to focus your attention in order to heal the gut and deal with some of the system problems that arise from gut pathology.
So let’s look at each of these in a little more detail.
1. Low Stomach Acid (Hypochlorhydria & bile/enzyme insufficiency)
The stomach produces hydrochloric acid, which is stomach acid, and it serves three primary functions:
- The chemical breakdown of food
- The absorption of nutrients
- Protection against pathogens
Bile (stored within the gallbladder) and other digestive enzymes created by the pancreas also play a major role in the way our body is digesting and absorbing nutrients.
Bile helps us to break down fat and enzymes help us break down protein, fat, and carbohydrate. So if the secretion of hydrochloric acid or bile or enzymes or all of the above is impaired, then that’s going to lead to problems all the way down the digestive tract.
2. Small Intestinal Bacterial Overgrowth (SIBO)
A poor diet, low stomach acid, antibiotic use, acid-suppressing drugs, impaired function of the migrating motor complex (MMC), constipation, gut infections, structural abnormalities of the GI tract, and immune dysfunction are all risk factors associated with small intestinal bacterial overgrowth.
This is a condition where you have overgrowth of bacteria in the small intestine, which then leads to several dysfunctions, including:
- decreased vitamin/mineral absorption (anemia, neuropathy, energetic problems, etc.)
- carbohydrate malabsorption
- excessive gas production (bloating, constipation, diarrhea)
- decreased fat absorption
- decreased protein absorption
- Intestinal permeability (leaky gut)
- Autoimmunity
3. Infections (parasites, pathogenic bacteria, fungal overgrowth)
The world of parasites is interesting. To start, not everyone with the same parasite will have problems because of it. Ultimately, it simply depends on the individual’s current health status and immune function.
The primary risk factors of parasitic infections causing problems in your body include consuming contaminated food and water, increased use of
daycare centers, travel to developing countries, household pets, consumption of uncooked foods, antibiotic use, insect vectors, and sexual contact.
Symptoms are often general and nonspecific. They vary from fatigue and malaise to GI distress, diarrhea, and constipation to things like brain fog, sleep disturbance, or skin issues.
In addition, I have found that many patients don’t exhibit digestive symptoms but present with other cyclical symptoms because parasites have lifecycles that can influence their pathogenicity in the host.
So one red flag for parasitic infection is if someone feels relatively normal and then they feel really kind of rotten and then they feel normal again, and that
alternates consistently.
4. Dysbiosis (Imbalances in Good vs Bad bacteria)
Dysbiosis is a situation where there’s an underrepresentation of beneficial microbes and an overrepresentation of harmful microbes.
For example, Candida is a normal resident of the human gastrointestinal tract. However, Candida can become overrepresented when levels of beneficial microbes that protect against that colonization are low.
They have shown Candida colonization to promote low-level inflammation, delay healing of inflammatory lesions, and potentially elevate levels of pro-inflammatory cytokines like interleukin 17.
Overall host immune status and the body’s own ability to protect against unfavorable overgrowth also influence gut dysbiosis and fungal overgrowth.
Symptoms range from obvious things like gastrointestinal discomfort to less obvious symptoms like depression, anxiety, brain fog, ADHD, autism spectrum disorder, skin disease, neurological problems, etc.
5. Food Sensitivity & Intolerances
Most times, food intolerances are a consequence of other pathologies, such as disrupted gut microbiome, SIBO, or intestinal permeability.
However, food intolerances can also cause problems like intestinal permeability. Therefore, food intolerance needs to be addressed independently.
Individual food intolerances can be severe. Others may be less severe but cause chronic low-grade inflammation and intestinal permeability, which can then lead to antibody production in everything from the joints to the myelin sheath in the brain, and certainly over time can lead to more serious pathologies and disease.
One thing to know about food sensitivity or intolerance testing is that every single test is based on immune function. If your immune cells are low, the food sensitivity test may be inaccurate. In addition, if you have major gut infections, food sensitivity is going to be inaccurate.
6. Intestinal Permeability (Leaky Gut)
Respected researcher Dr. Alessio Fasano, who is well known for his discovery of zonulin, a protein that regulates tight junction permeability, believes that leaky gut is actually a precondition to developing autoimmunity, along with genetic vulnerability and environmental triggers.
He has argued that increased permeability of the intestinal barrier to macromolecules is associated with local and systemic inflammatory conditions, including, of course, celiac and non-celiac gluten sensitivity, food intolerances, IBD, many autoimmune diseases, neurological conditions like MS, cognitive dysfunction, behavioral disorders, skin conditions, and new connections that we’re discovering.
7. Autoimmunity
There are more than 80 different autoimmune diseases currently known.
Multiple sclerosis, type 1 diabetes, and rheumatoid arthritis all fall under this category, and even thyroid disorders are usually attributable to autoimmunity.
A variety of health factors likely play a role in these chronic illnesses, including the gut microbiome and intestinal permeability.
Risk factors include: Genetics, cigarette smoking, diet, physical inactivity, obesity, infections, antibiotics, NSAIDs, oral contraceptives, chronic stress, and sleep deprivation.
The Brain-Gut Axis and Neuroinflammation
90% of the brain is immune cells, with neurons making up the remaining 10 percent.
Our bodies have an incredible ability to protect and heal themselves through the process of inflammation.
Inflammation is the body’s defense mechanism against harm, injury, and infection and is ultimately controlled by the immune system.
If most our immune system is within the digestive system, then making the connection between brain based disorders and GI disorders is paramount.
While inflammation is well intended in protecting our bodies, this reaction is not always good for our health.
Our bodies often view added chemicals or artificial ingredients found in food, environmental toxins and pollutants as infectious, inducing a mild inflammatory response.
This happens particularly in the gut, where these substances are broken down and digested. Over time, consistent exposure to these minor toxins leads to chronic low-grade inflammation which does not affect daily function, but can lead to negative health outcomes. We have associated chronic inflammation with depression, anxiety, arthritis, cancer, neurodegenerative conditions, heart and neurological disease.
When chronic inflammation occurs in the gut specifically, our brains are in danger.
The gut is full of nerve endings which together make up the enteric nervous system (ENS). The central nervous system, controlled by our brains, is connected to the ENS through the vagus nerve, which runs from the medulla of the brainstem to the gut.
This relationship is often referred to as the gut/brain connection and through it, information collected by the nerves in your gut is communicated directly to the brain, inducing an inflammatory response.
Chronic inflammation of the gut leads to neuroinflammation, or inflammation of the brain and nervous tissue. This can trigger neurodegenerative diseases, such as alzheimers, Parkinsons and ALS, as well as generalized anxiety disorder.
It is well appreciated that gut microbiome (and neuroinflammation) play a key role in visceral or abdominal pain, their roles in other types of chronic pain have only been recently acknowledged including:
- inflammatory pain
- neuropathic pain
- headache, and opioid tolerance
Therefore, the health of our gut not only affects our mood and the way we think and feel, but also our long-term brain health and risk of developing serious disease and chronic pain.
Testing for Underlying Digestive Dysfunctions
In order to overcome digestive disorders, a thorough history, functional blood chemistry or advanced lab testing and a comprehensive stool test are an excellent start.
Unfortunately, many patients with digestive issues start with imaging studies such as endoscopic procedures, CT scans and barium swallows, or enemas.
While it’s great to rule out serious pathology and disease, unfortunate truth is these types of diagnostics rarely lead to an accurate diagnosis, much less effective treatment plan.
Functional Blood Chemistry Testing
Most doctors are routine with their lab testing. They order enough testing to make sure you will not drop dead tomorrow, but not nearly enough to accurately assess health.
A good functional lab testing panel will appropriately evaluate the following systems:
- Blood Sugar Regulation
- Thyroid Function
- Cardiovascular Risk
- Adrenal Function
- Kidney Function
- Red Blood Cell Function
- GI Function
- Gallbladder Function
- Immune Function
- Liver Function
- Bone Health
In addition, there are blood chemistry markers that allow for the observation of problems, including:
- Inflammation status
- Oxidative stress
- Heavy metal or Toxic Load
- Digestion and absorption of macronutrients (protein, carbs, fats)
- Vitamin and Mineral absorption potential
- Actual vitamin and mineral status
All together, if you understand how to interpret blood chemistry appropriately, this is a major start with understanding what could drive your health issues.
Beyond blood chemistry testing, we’d then consider comprehensive stool testing.
Comprehensive Stool Testing
There are many tests out there, but not all of them are the same.
So if you get any microbiome testing, make sure it’s with an appropriate lab and make sure they give you proper prep instructions for getting the most accurate results.
A comprehensive stool panel will
- quantify your microbiome (good vs. bad bacteria)
- assess for parasitic infections, fungal overgrowth, and viral infections.
- screen for your ability to digest and absorb nutrients
- assess for immune function and inflammation, specifically within the digestive system
Advanced Digestive Health Testing
Honestly, a thorough health history and intake, comprehensive blood chemistry testing and stool testing should all be enough to address the vast majority of digestive dysfunctions.
If you’re not able to come to a resolution, additional testing could include:
- Food Sensitivity Testing
- Small Intestinal Bacterial Overgrowth Testing
- Organic Acid or metabolomic testing
- Toxicity Testing