Can Your Gut Cause Joint Pain?
Even Hippocrates, the father of modern medicine, said all healing begins in the gut!
And more than 2,300 years later, we are just beginning to unravel the importance of the microbiome (collection of bacteria in your gut) and it's relationship to weight loss, brain chemistry, hormone balance, autoimmunity and yes… joint pain.
When it comes to treating musculoskeletal conditions, it's important to appreciate the role that your diet can play in the development of inflammation and pain.
In fact, for anyone experiencing any type of joint pain, I would challenge them to eliminate the following foods for at least 30 days:
- Grains
- Corn
- Soy
- Dairy
- Alcohol/Smoking/Sugar
I bet you'll fee better.
As a doctor of chiropractic and a functional medicine practitioner, I spend quite a bit of time studying gut health and how it leads to obesity and weight gain; which also directly contributes to the development of osteoarthritis in weight-bearing joints.
While it's not far fetched to understand how poor eating choices can contribute to weight gain or poor digestion, most of you would likely never make the connection between gut health and joint pain, or even other problems such as headaches, mood swings, eczema and fatigue.
But they are absolutely all connected and if you have any of the above mentioned problems or conditions, you should absolutely consider improving your gut health.
How Your Gut Contributes to Joint Pain
When doctors treat arthritis, they often recommend medications, physical therapy, exercise, and losing weight, but they rarely recommend eliminating or adding specific foods to a diet.
However, research suggests that diet can impact the inflammation that causes arthritis pain, including pain from rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and other diseases. [1]
In order to really understand this, you need to understand the following concepts:
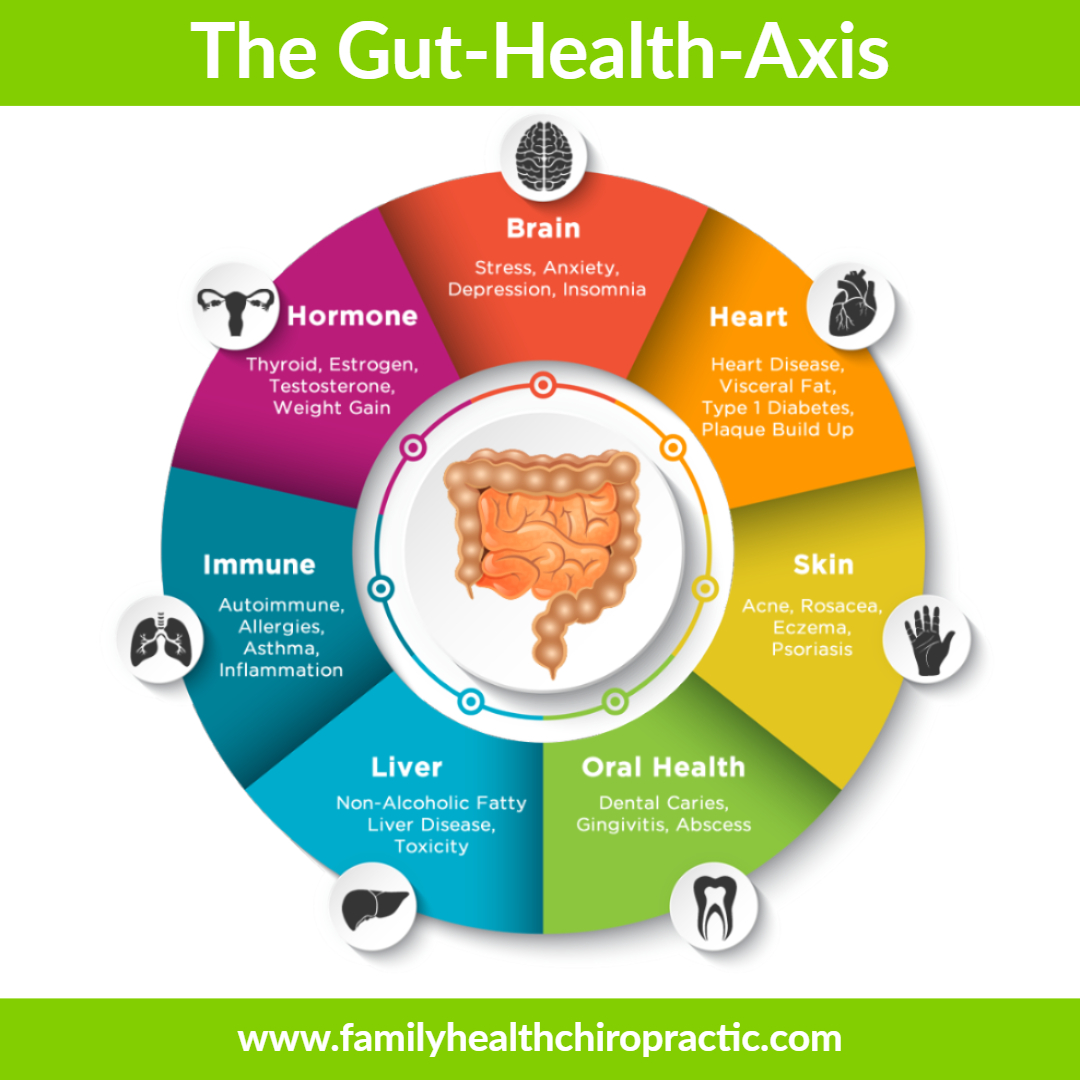
The Gut-Health-Axis Impacts Overall Health
I've written about Gut Health extensively on my Functional Medicine website. Whether it's mood disturbance, depression, anxiety, hormone imbalance, liver problems or heart health; everything is connected to the Gut! Imbalances in the gut microbiome (good vs bad bacteria) is also associated with any chronic inflammatory disease, including the various forms of arthritis.
The Diet Influences the Gut Microbiome
There's no way around it – you have to improve your diet! There's no pill, potion or lotion. Not even colonics or bowel flushing will balance the microbiome. [2] A gut microbiome’s diversity and balance of species are all directly influenced by diet. The best diet for your microbiome is diversity in the amount of plants, fruits and vegetables that you eat.
The Gut Microbiome Can Trigger Inflammation
The short version of this story involves imbalances in the good versus bad bacteria in your gut (dysbiosis), which then triggers inflammation. [3] This inflammation then leads to a leaky gut which results in inflammation of the liver.[5] This process is made worse by the fact that there is a direct route from the Gut to the liver, known as the portal vein. The portal vein then allows undesirable content in the gut to be deposited directly into the liver, contributing to more inflammation and congestion. It's a vicious cycle that prevents your body from properly detoxing and eliminating dangerous waste products.
Over the last few years, researchers have linked unhealthy guts or dysbiosis with joint pain [6], rheumatoid arthritis [7] and osteoarthritis [8].
Reduce Joint Pain by Healing Your Gut
I've analyzed several hundred stool panels and cannot tell you how many interesting things were discovered.
First and foremost, it's safe to say that almost everyone has some level of dysbiosis.
I've only ever seen a few individuals who had healthy levels of “good bacteria”.
Short from getting a comprehensive stool panel done, here's a few things you can do right now to improve gut health:
1. Follow a 30-day Paleo Reset diet
I'd start by following a 30-day Reset Diet that includes high-quality, natural animal meats, bone broths, eggs, starchy and non-starchy vegetables, fermented vegetables, traditional fats, sea salt, and spices.
During this reset period, the following foods are completely off-limits: dairy, grains, sweeteners, sodas, legumes, processed foods, alcohol, and industrial seed and vegetable oils.
After 30 days, you'd reintroduce ‘gray-area' foods into the diet to figure out safe and unsafe foods for regular consumption.
For persistent digestive symptoms that don’t resolve, add these modifications:
- Reduce your intake of non-starchy vegetables that are high in insoluble fiber, and prepare them with methods designed to make them more digestible (including fermentation) when you do eat them.
- Avoid or greatly restrict foods that are high in FODMAPs.
- Consume between one-half and one cup of bone broth per day, in soups, stocks, stews, or sauces. You can also drink it like tea.
- If you have GERD, heartburn, or inflammatory bowel disease, you may need to follow the GAPS diet and limit starchy foods for a period of time.
- Eat fermented foods like sauerkraut, kimchi, cortido (Salvadoran sauerkraut), beet kvaas, kefir (dairy or water), and yogurt. Though milk (in kefir and yogurt) and cabbage (in sauerkraut and kimchi) are both high in FODMAPs, fermentation breaks them down and makes these foods tolerable for most people with digestive issues.
- Limit alcohol consumption to four to six drinks per week, or remove it altogether.
2. Address your stress level
Consider mindfulness-based stress reduction or gut-directed hypnotherapy (especially for IBS).
3. Optimize sleep quality
In addition to managing stress, improving sleep quality and making sure your patients get enough sleep are also important. Disturbed sleep interferes with gut functions in several ways.
4. Consider Gut Health Supplements
If you shows signs of maldigestion, take betaine hydrochloric acid and/or a blend of digestive enzymes containing acid-stable proteases, pancreatin, bromelain, and ox bile.
5. Restore the gut barrier
L-glutamine, N-acetyl glucosamine, MSM, quercetin, mucin, DGL, slippery elm, marshmallow, and chamomile are all helpful.
6. Repopulate the gut microflora with broad-spectrum probiotics
Start at a low dose and build up slowly over time to avoid negative reactions. Patients with SIBO may not tolerate probiotics with acidophilus and they may not tolerate prebiotics, even at low doses.
Final Thoughts
Many digestive disorders originate from a short list of underlying imbalances in the gut and these imbalances can then cause all sorts of chronic health problems.
Almost all digestive disorders share one or more of the following underlying mechanisms:
- An overgrowth of bacteria in the small intestine
- An imbalance between “good” and “bad” microbes in the gut
- A permeable gut barrier (leaky gut)
- Chronic bacterial, parasitic, or fungal infections (such as pylori, Blastocystis hominis, Candida albicans)
- Low stomach acid or digestive enzyme production
- Sensitivity, allergy, or intolerance to certain foods
- Impaired communication between the gut and the brain
Tweaking the diet, addressing maldigestion, healing the gut lining, replenishing the gut microflora, and managing stress can improve gut health and function and ultimately impact systemic inflammation including arthritis and joint pain.