Different Types of Headaches
When it comes to headaches, there are two categories: Primary Headaches and Secondary Headaches.
Primary headaches are any form of headache that is not caused by a serious medical condition. These types of headaches include: migraine, cluster, trigeminal and tension headaches.
Secondary headaches are headaches caused by some other health disorder or medical condition.
Examples include fever, infection, overuse of medication, stress or emotional conflict, high blood pressure, psychiatric disorders, head injury or trauma, stroke, tumors, and nerve disorders.
If you suffer from migraines, you're not alone!
Migraines are the third most prevalent illness in the world and currently, 25% of US households have someone who currently has regular attacks.
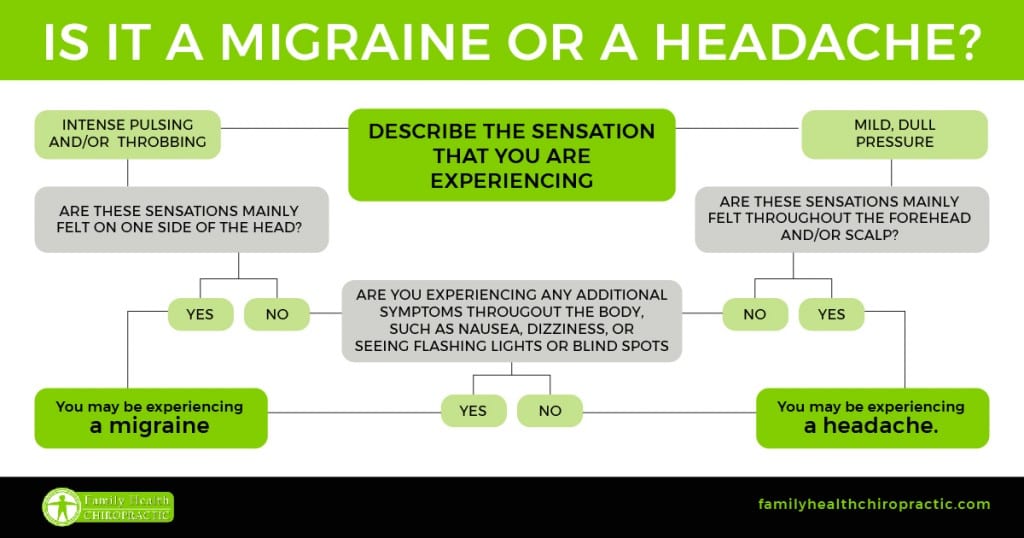
How to Determine if You Have Migraine Headaches
Migraine headaches can lead to pounding pain, light as well as sound sensitivity, nausea and digestive problems and an overall decrease in one's quality of life.
Classic symptoms of migraine headaches include:
- Intense or severe pounding pain on one or both sides of the head — most people have migraine pain on only side of the head at a time, which is a symptom that makes migraines different from tension or cluster headaches
- Nausea, loss of appetite or an upset stomach (sometimes even vomiting)
- Increased sensitivity to sound and light
- Irritability
- Disturbed or blurred vision, seeing flashing lights, or seeing unusual shapes and lines (especially while an attack is just starting)
- Dizziness and shakiness
- Numbness or weakness in the facial or neck muscles
- Increased thirst
- Inability to concentrate, speak normally or hold a conversation
Most people who suffer from migraines claim that they can tell when a migraine is about to occur. Most patients state that they just feel “off” and sometimes experience “auras” or “visual disturbances”.
Most people will also experience their migraines about once or twice a month, but others will get them every single day, for several days in a row.
The Phases of a Migraine
Migraine headaches can be divided into four phases, all of which may be present during the attack:
- Premonitory symptoms occur up to 24 hours prior to developing a migraine. These include food cravings, unexplained mood changes (depression or euphoria), uncontrollable yawning, fluid retention, or increased urination.
- Aura. Some people will see flashing or bright lights or what looks like heat waves immediately prior to or during the migraine, while others may experience muscle weakness or the sensation of being touched or grabbed.
- Headache. A migraine usually starts gradually and builds in intensity. It is possible to have migraine without a headache.
- Postdrome (following the headache). Individuals are often exhausted or confused following a migraine. The postdrome period may last up to a day before people feel healthy.
Who Gets Migraine Headaches?
A number of different factors can increase your risk of having a migraine.
These factors, which trigger the headache, vary from person to person and include:
- inflammation that affects normal blood flow and the blood vessels
- changes in nerve signals and brain chemicals that cause pain
- activation of the trigeminal nerve (which releases substances that signal pain to the brain)
- sudden changes in weather or environment
- too much or not enough sleep
- strong odors or fumes
- emotion, stress or overexertion
- loud or sudden noises
- motion sickness
- low blood sugar
- skipped meals
- tobacco
- depression and/or anxiety
- head trauma
- hangover
- over use of medications or side effects of medications
- hormonal changes
- genetic susceptibility (strong research exists to support a genetic component)
In some 50 percent of migraine sufferers, foods or ingredients can trigger headaches.
These include aspartame, caffeine (or caffeine withdrawal), wine and other types of alcohol, chocolate, aged cheeses, monosodium glutamate, some fruits and nuts, fermented or pickled goods, yeast, and cured or processed meats.
Migraines can occur in both children and adults, but affect adult women three times more often than men.
When it comes to migraines in women and hormone fluctuations, it's common to find that the migraine may begin at the start of the first menstrual cycle or during pregnancy. Most women see improvement after menopause, although it's also been observed that surgical removal of the ovaries can worsens migraines. Women with migraine headaches who take oral contraceptives may experience changes in the frequency and severity of attacks, while women who do not suffer from headaches may develop migraines as a side effect of oral contraceptives.
Medical Treatment of Migraine Headaches
Migraine symptoms are commonly managed with medications that help reduce pain and inflammation. Drugs used to control migraines can be classified into Acute and Preventive treatments. Preventive treatment involves taking medicines daily to reduce the severity of future attacks or keep them from happening at all.
Acute treatment for migraine may include any of the following drugs:
- Triptan drugs increase levels of the neurotransmitter serotonin in the brain. Serotonin causes blood vessels to constrict and lowers the pain threshold.
- Ergot derivative drugs bind to serotonin receptors on nerve cells and decrease the transmission of pain messages along nerve fibers. They are most effective during the early stages of migraine and are available as nasal sprays and injections.
- Non-prescription analgesics or over-the-counter NSAID drugs such as ibuprofen, aspirin, or acetaminophen can ease the pain of less severe migraine headache.
- Nausea relief drugs can ease queasiness brought on by various types of headache.
- Narcotics are prescribed briefly to relieve pain. These drugs should not be used to treat chronic headaches.
Preventive treatment for migraine may include any of the following drugs:
- Anticonvulsants may be helpful for people with other types of headaches in addition to migraine. Although they were originally developed for treating epilepsy, these drugs increase levels of certain neurotransmitters and dampen pain impulses.
- Beta-blockers are drugs for treating high blood pressure that are often effective for migraine.
- Calcium channel blockers are medications that are also used to treat high blood pressure treatment and help to stabilize blood vessel walls. These drugs appear to work by preventing the blood vessels from either narrowing or widening, which affects blood flow to the brain.
- Antidepressants are drugs that work on different chemicals in the brain; their effectiveness in treating migraine is not directly related to their effect on mood. The types of antidepressants used for migraine treatment include selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors, and tricyclic antidepressants (which are also used to treat tension-type headaches).
Taking headache relief drugs more than three times a week may lead to medication overuse headache (previously called rebound headache), in which the initial headache is relieved temporarily but reappears as the drug wears off.
Taking more of the drug to treat the new headache leads to progressively shorter periods of pain relief and results in a pattern of recurrent chronic headache. Headache pain ranges from moderate to severe and may occur with nausea or irritability. It may take weeks for these headaches to end once the drug is stopped.
Are these medications always necessary, safe and effective?
No, not always. Research shows that holistic, non-drug strategies can also play an important role in managing pain and preventing headaches. The best part is that improving your diet and lifestyle habits also benefits your health in many other ways and doesn’t pose the same risks that drugs do.
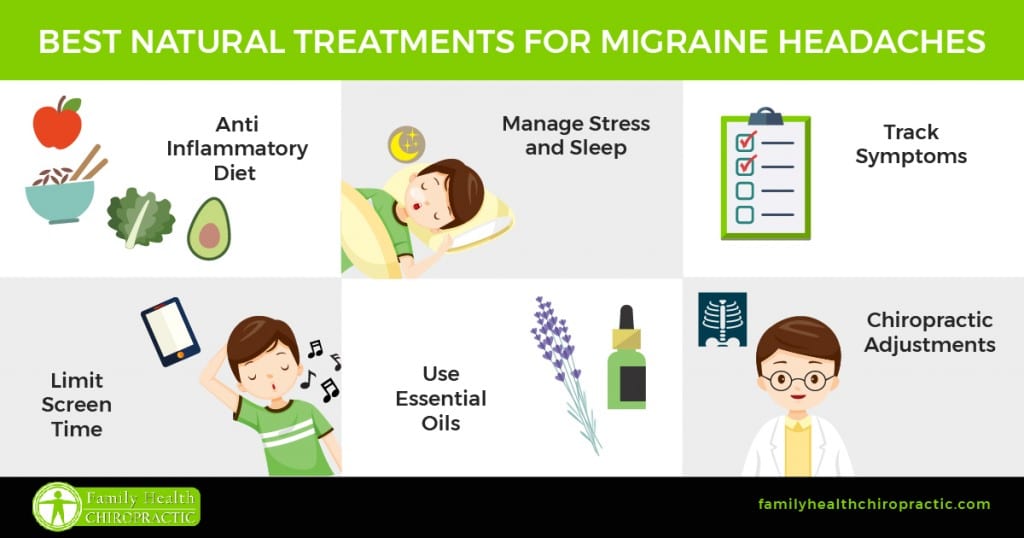
Natural Treatments for Migraine Headaches
Eat an Anti-Inflammatory Diet
Everybody knows that a poor diet contains large amounts of processed foods (which contain large amounts of sodium). Processed food is one of the biggest triggers for migraine symptoms.
Foods that can make migraine headaches much worse include added sugar, refined grain products, conventional dairy products, aged cheese, red wine, chocolate, eggs, artificial food additives (such as msg or aspartame), flavor enhancers, high amounts of sodium, very cold foods or nitrates in processed meat.
Foods that can help prevent or treat migraines include those with omega-3 fatty acids (like nuts, seeds and wild-caught fish or grass fed beef), fresh fruits and vegetables and other healthy, lean proteins.
Manage Stress and Get Enough Sleep
Not getting enough rest or recovery time can increase the instance of migraines. Stress hormones can also cause problems by impacting blood flow which then causes headaches.
Make an effort to stick to a regular sleeping schedule and make sure that you're taking enough time out of your day to focus on stress reducing activities such as exercise, reading, deep breathing, yoga, tai chi, walking outdoors and meditation.
Keep a “Migraine Journal” to Track Symptoms
One of the best tools at your disposal is a journal. With so many factors that can contribute to migraine headaches, keeping a journal of when your headaches occur and writing down what you've been doing; you might be able to pinpoint an actual cause or trigger.
It could be your diet, nutrient deficiencies (such as magnesium deficiency), exercise routine or other factors.
Limit Screen Time or Lots of Light Exposure
If you notice that migraines are triggered from blue light exposure being omitted from electronic devices, limit the amount of time you spend using these devices or consider wearing blue light-blocking glasses. If sunlight seems to worsen headaches, wear sunglasses when outdoors (especially those that are tinted blue or green to block UV rays reaching your eyes).
Use Essential Oils and Heat
Essential oils for headaches include peppermint, lavender, eucalyptus, frankincense and rosemary. These can be applied to the painful side of the head, neck and elsewhere to soothe tension and stress.
You can also numb the pain with a heated towel, heating pad or ice pack applied to the head, upper back or neck for about 15 minutes at a time.
Chiropractic Adjustments & Spine Alignment
Studies have found that migraines can be caused by a small misalignment in the spine. When your vertebrae are misaligned in this way, it can actually cause the nerves and muscles to become irritated and inflamed.
When you get a chiropractic adjustment, this misalignment is corrected, meaning your vertebrae are where they should be.
Chiropractic adjustments are not only great for helping reduce the severity of migraines, but regular chiropractic care can also help reduce the frequency of these migraines as well.
In addition, many migraine sufferers may not realize that their poor posture can be contributing to their migraines as well. When you spend the whole day hunched over a phone, tablet or computer screen, you start putting some serious strain on your neck and back muscles, which can increase inflammation of the nerves and tissue that are associated with migraine headaches.