Thousands of years ago, humans were simple hunter/gatherers. Our diet consisted of fruits, nuts, tubers and the occasional feast of meat. But eventually, we learned to cultivate plants, and the agricultural revolution was born. And as our eating habits changed, some unanticipated problems certainly arose. Considering that the human gut took 2 million years to develop, this sophisticated organ came to tolerate foods that were staples of the human diet. But with the sudden change brought on by the agricultural revolution, how would it react to new foods instantly appearing in the diet?
If one were to study the fossil record and compare homo sapiens pre and post agricultural revolution, you'd find skeletons that show a sharp decline in stature (as much as 6 inches from male specimens), with modern populations still yet to regain the height of their distant ancestors. But the most compelling evidence has come from Archaeological studies by the University of Massachusetts who show early farmers paid a price for their new-found livelihood. Compared to the hunter-gatherers who preceded them, the farmers had a nearly 50 per cent increase in enamel defects indicative of malnutrition, a fourfold increase in iron-deficiency anemia (evidenced by a bone condition called porotic hyperostosis), a theefold rise in bone lesions reflecting infectious disease in general, and an increase in degenerative conditions of the spine, probably reflecting a lot of hard physical labor.
“Life expectancy at birth in the pre-agricultural community was bout twenty-six years, but in the post-agricultural community it was nineteen years.”
So these episodes of nutritional stress and infectious disease were seriously affecting their ability to survive. What we now know is that the agricultural revolution that occurred roughly 10,000 years ago generated a whole battery of food proteins previously unknown to the human gut, including proteins from cow, goat, and donkey milk, as well as birds’ eggs and cereals. While most individuals were able to adapt, those who could not developed food intolerance's (where food acts as a toxin) and serious diseases including Celiac Disease (CD) was born. So Celieac Disease, Food Intolerance (food acting as toxins) and Food Allergies are not modern afflictions.
About 8000 years after CD was born, a clever Greek physician named Aretaeus of Cappadocia, living in the first century AD, wrote about “The Coeliac Affection.” In fact, he named it “koiliakos” after the Greek word “koelia” (abdomen). His description: “If the stomach be irretentive of the food and if it pass through undigested and crude, and nothing ascends into the body, we call such persons coeliacs”. (1) But neither Aretaeus nor anyone else knew that CD was caused by an autoimmune reaction to gluten, a protein in wheat. It wasn’t until several centuries later – in the 1950s — when Dr. Willem Dicke, a Dutch pediatrician, conclusively proved that gluten was the culprit. (2) Dicke’s discovery saved millions of children and adults from the perils of untreated celiac disease, including malnutrition, stunted growth, cancer, severe neurological and psychiatric illness, and even death.
Since then, the majority of our understanding of gluten intolerance has been relatively simple: Either you have Celiac Disease, meaning just a small bit of gluten will send you running to the bathroom, or you don’t, and you’re somehow allowed to down bagels and beer without fear. But modern science has a different perspective and has even demonstrated that many of us have “Non-Celiac Gluten Sensitivity” (i.e. people that react to gluten but do not have Celiac Disease).
What I hope to help you understand is that just because you don't have digestive disturbance or poop problems, doesn't necessarily rule out sensitivity. This is very, very important considering that the gluten protein has impact not only on your intestinal system, but your skin, immune cell and even brain cells. So gluten reactions can show up in all sorts of ways and may take years to develop symptoms.
The Many Faces of Gluten Intolerance
To help you understand how you can be gluten intolerant without having Celiac Disease or GI disturbance, we need to cover some basic biochemistry of wheat components and wheat digestion.
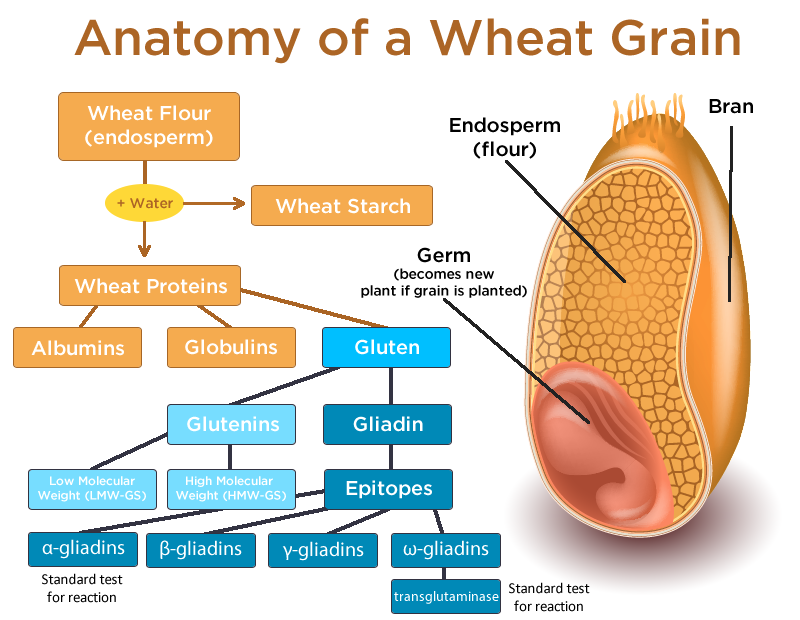
Wheat contains several classes of proteins called albumins, globulins and gluten. Gluten can be further broken down to Glutenins and Gliadins. (They basically give your bread the ability to rise and become gooey.) Within the gliadin class, there are four different epitopes (i.e. types): alpha-, beta-, gamma- and omega-gliadin. Wheat also contains agglutinins (proteins that bind to sugar) and prodynorphins (proteins involved with cellular communication). Once wheat is consumed, enzymes in the digestive tract called tissue transglutaminases (tTG) break down the wheat compound. In this process, additional proteins are formed, including deamidated gliadin and gliadorphins (aka gluteomorphins).
Here’s the important thing to understand: Celiac Disease or Gluten Intolerance is currently diagnosed as a response to one specific type of gliadin (alpha-gliadin) and a specific type of transglutaminase (tTG-2). BUT… we now know that people react to other components of wheat and gluten — including other types (beta, gamma, omega), glutenins and other types of transglutaminases, including type 3 (primarily found in the skin) and type 6 (primarily found in the brain). (3, 4, 5, 6, 7)
This is a major problem in the case of misdiagnosis when it comes to conventional lab testing for Celiac Disease and Gluten intolerance. Most doctors only test patients for antibodies to alpha-gliadin and transglutaminase-2. If you’re reacting to any other parts of the wheat protein (e.g., beta-gliadin, gamma-gliadin or omega- gliadin), or any other types of transglutaminase (e.g., type 3 or type 6), you’ll test negative for these conditions regardless of how severely you’re reacting to wheat. To make matters more complicated, you need to distinguish between a “Gluten Sensitivity” and “Wheat Allergy” – and both are different.
Celiac Disease is Only Part of the Problem
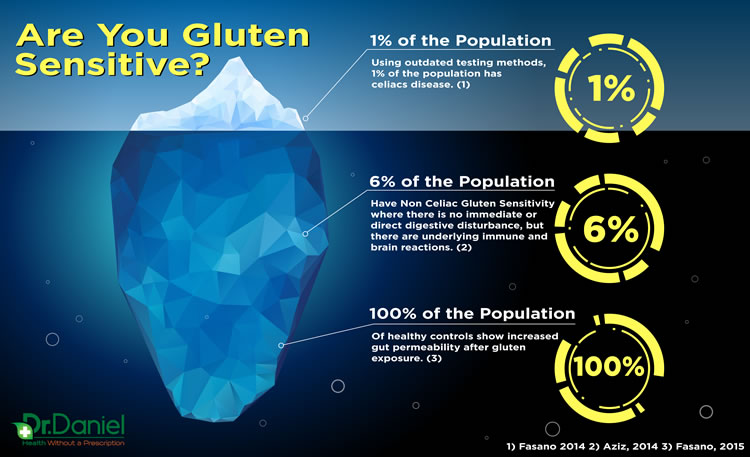
According to the most recent large scale study, Celiac Disease affects between .7 percent and 1 percent of the U.S. population. (8) However, considering that most physicians rely on the limited scope of conventional testing, the actual incidence is likely much higher. It's just not being diagnosed properly.
That said, Celiac disease is only part of the problem of a bigger picture. When it comes to gluten intolerance, there are many possibilities of expression – not simply an autoimmune reaction as is the case with celiac disease. And currently, all of the other forms of gluten intolerance are collectively known as “non-celiac gluten sensitivity” or NCGS.
Also the current definition of NCGS is still being debated and we certainly no that there are many forms or conditions that “resolve when gluten is removed from the diet and CD and allergy have been ruled out.” (9)
Gluten Intolerance Is More Common Than Currently Estimated
In 2015, the estimation for the number of people affected by non-celiac gluten sensitivity ranged between .5 percent and 13 percent. (10) In the next few paragraphs I’m going to try and explain why this number is quite small and how likely it is that we are “low-balling” it.
Let me start by stating the obvious: it’s nearly impossible to estimate the prevalence or occurrence of Non-Celiac Gluten Sensitivity because there is no definitive diagnostic tool. Remember, the only tests available are for alpha-gliadins and transglutaminase. In addition, even the best blood chemistry labs are not 100% accurate. So to date, the only way to truly know if you are gluten sensitive in any way is to eliminate gluten from your diet for a period of 60-90 days. This is by far the gold standard for diagnosing gluten intolerance. However, many physicians are unaware of this and thus do not suggest it to their patients.
The other problem is that of misdiagnosing due to the wide variety of symptoms caused by celiac disease and NCGS. Gluten is certainly often coupled with symptoms of GI distress and discomfort leading many “GI” physicians and patients to only suspect gluten when digestive symptoms are present.
However, both gluten intolerance and celiac disease can be present in the absence of gut distress and only manifest with symptoms like ataxia (loss of muscle control), schizophrenia, dermatitis (skin irritation), or neuropathy (nerve damage). In fact, it has been demonstrated that the majority of patients with neurological problems due to gluten sensitivity have absolutely no gastrointestinal symptoms! (11)
Even in the case of celiac disease, which has more solid research than Non-Celiac Gluten Sensitivity, 30 percent of newly diagnosed patients do not have gut symptoms, and for every new case that is diagnosed, there are 6.4 cases that are undiagnosed—the majority of which are atypical or “silent” forms without gut symptoms. (13, 14)
Truth is, if your sensitive to any components of gluten, it can affect nearly every tissue in your body, including the:
- Brain
- Skin
- Endocrine system
- Stomach
- Liver
- Blood vessels
- Smooth muscles
- and even the nucleus of cells
This means that Celiac Disease and Non-Celiac Gluten Sensitivity are associated with a wide variety of disease such schizophrenia, epilepsy, Type 1 diabetes, osteoporosis, dermatitis, psoriasis, Hashimoto’s hypothyroidism, and peripheral neuropathy. (15) And herein lies the problem- gluten will not be suspect in a patient for these conditions, because both doctors and patients only consider CD and NCGS when there’s gut problems.
Thinking “Gluten Free” is Just a Fad is Downright Dangerous
Despite the large collection of evidence that now exists to support Non-Celiac Gluten Sensitivity, mainstream media and medical professionals continue to declare the need to go “Gluten-Free” is just a fad. Making things worse, it’s not uncommon to see major headlines from popular media sites suggesting NCGS is a myth! Even popular talk show hosts such as Jimmy Kimmel Live have gotten in on the mis-information that “science journalism” often gets so wrong.
Research Confirms Gluten Intolerance is real— and likely affects 50-90% of the popluation.
And while I can certainly relate to an aversion of fads (don’t get me started with diets and hipsters and Skinny Jeans), the scientific community is clear when it comes to Non-Celiac Gluten Sensitivity being a legitimate condition. I would love someone to conduct a study to observe the wrecklessness and sheer devastation that “lame-stream media”, would be scientist reports of “Science Journalism” and ignorant “Medical professionals” cause towards misinformed consumers.
Statistics show that an estimated 75-90% of the population have been impacted by food intolerances and sensitivities. Research indicates that Leaky Gut Syndrome affects millions of people worldwide. Leaky Gut Syndrome is a chronic debilitating condition that often goes undiagnosed by most mainstream medical professionals. Of course this is a huge concern considering that conventional medical professionals don't believe this condition even exists. As a result; many people are not aware that the sufferings and symptoms they are presently dealing with are being caused by the Leaky Gut they have developed over time. We need to emphasize this problem is very real and even more importantly we need to understand how to stop it's progression.
Test, Don't Guess
By now you should understand that there are certain individuals (possibly yourself) who possess non-celiac wheat sensitivity and would benefit greatly from avoiding wheat and related gluten containing foods. Look, I love Pizza, Hamburgers and gooey, chewy bread stuff… but not more than Alzheimers, Multiple Sclerosis or Intestinal Bowel diseases. I find it extremely unfortunate that so many people who might benefit from a gluten-free diet never try it, much less stick with it. I hope this article (and others that will surely follow) will make it just a bit easier for you and your family to make the right choice for their health.
I would certainly be suspicious if you or anyone you know:
- Have gut dysbiosis, which appears to be resistant to standard therapy
- Are suspected of having intestinal mucosal damage
- Complain of food allergy and intolerance
- Complain of chemical hypersensitivity
- Present multiple-symptom complaints (including Chronic Fatigue Syndrome and Fibromyalgia)
- Suffer from abnormal immune cell count and function
- May suffer from blood-brain barrier permeability, depression, or neuroautoimmunity
Additionally, It's imperative that you get checked if you are a Neuroautoimmune patient who has:
- Thyroiditis
- Arthritis
- Myocarditis
- Dermatitis
- Endocrinopathy
- Polyendocrinopathy
- Osteoarthritis
- Pernicious Anemia
How do you know whether you're at risk? There are two ways to determine your gluten tolerance:
- A Cyrex panel: Cyrex Array 3 is a panel that tests your potential for wheat and gluten protein reactivity and autoimmunity. It must be ordered by a healthcare practitioner and it costs $325. Know that is is my cost for ordering the test, I make no money from it (so no complaints). But considering the implications of knowing, is your health worth $325?
- A self-experiment: Eliminate gluten from your diet for 60 days and then perform a gluten challenge, taking careful note of any symptoms. I still hold that this is the best way to determine your tolerance for gluten.
BONUS: Here's a Digestive Health Quiz and my Gluten & Wheat Sensitivity Plan.
Now… I’d like to hear from you.
Did this article change your perception of gluten sensitivity?
Do you or someone you know have Non-Celiac Gluten Sensitivity?
Have you ever tried a gluten challenge?
Share your opinion in the comments or email me!